In May, 2023, the American College of Radiology (ACR) updated its guidelines for breast cancer screening, calling for earlier and more intensive testing for women with higher-than-average risk.¹
The new guidelines, which hadn’t been updated since 2018, now call for all women—especially Black and Ashkenazi Jewish women—to have risk assessment by age 25 to determine if screening earlier than age 40 is necessary. The ACR continues to recommend annual screening starting at age 40 for women of average risk, but earlier and more intensive screening for high-risk patients.
Other updates included:
- Women with genetics-based increased risk (including BRCA1 carriers), those with a calculated lifetime risk of 20% or more, and those exposed to chest radiation at a young age are recommended to have MRI surveillance starting at ages 25 to 30. These women should start annual mammography at ages 25 to 40, depending on the type of risk.
- Women diagnosed with breast cancer prior to age 50 or with a personal history of breast cancer, and dense breasts should have annual supplemental breast MRI.
- High-risk women who desire supplemental screening, but cannot undergo MRI screening, should consider contrast-enhanced mammography (CEM).
These new guidelines are based on the consensus of leading experts and provide radiologists with the support and direction that yields more informed decision making, and increases their opportunities to continue making meaningful differences in women’s lives through earlier breast cancer detection.
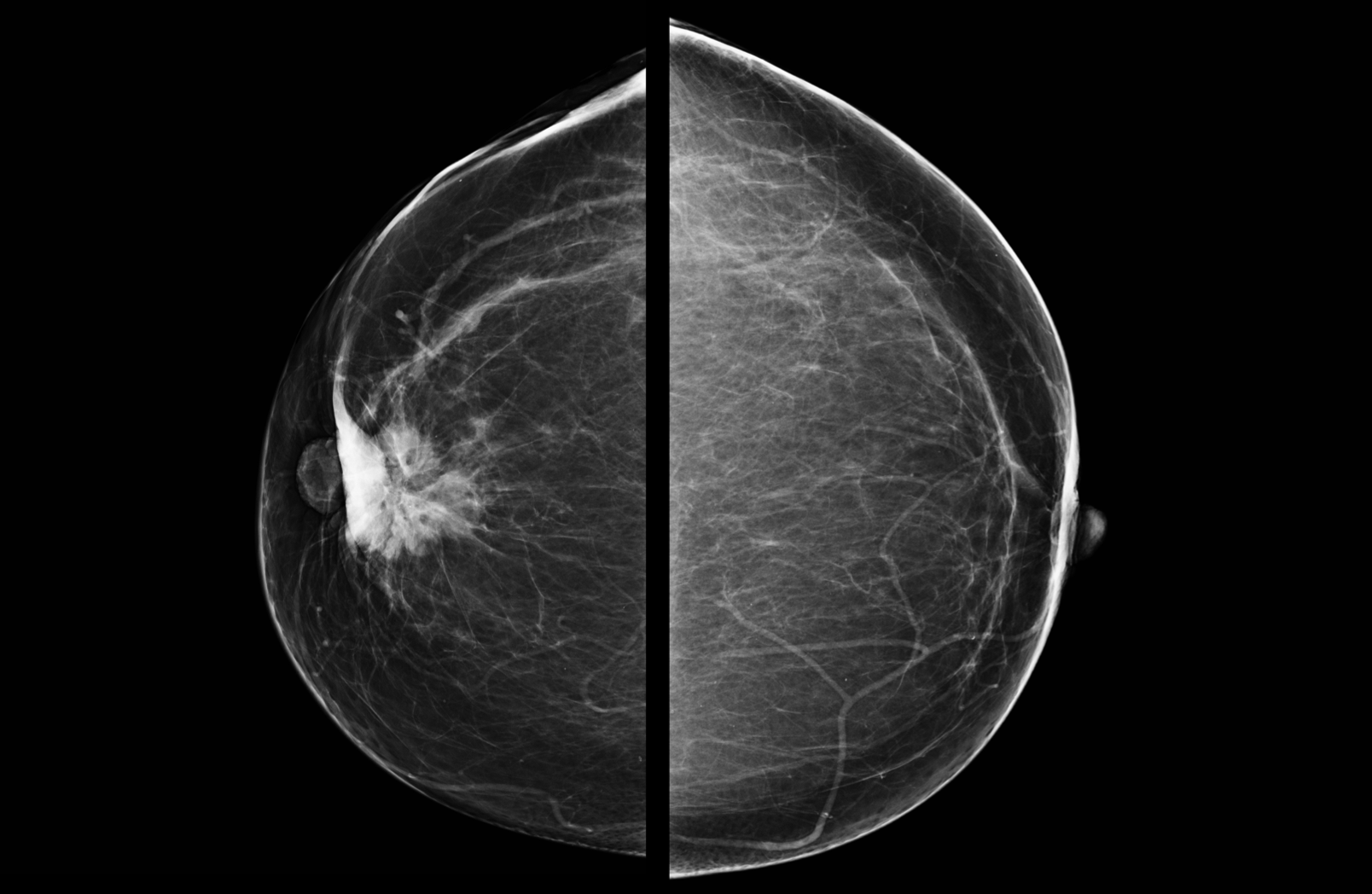
Images are for illustrative purposes only.
Helping Patients Decide to Pursue Supplemental Breast MRI
How do high-risk women decide whether or not to pursue supplemental screening with breast MRI? And how can you best facilitate the conversations that lead to these decisions, especially among patients who are at higher risk and may have trouble deciding?
Researchers at the University of Virginia have found an answer. A new paper published in the Annals of Surgical Oncology reported the results of a pilot program held at UVA Health which tested the use of an interactive decision aid designed for high-risk women who are considering supplemental screening with breast MRI.²
At the start of the program, among 24 participants, 16 women were undecided about pursuing a supplemental MRI screening.²
To help them decide, the new 3-part tool began with a segment that used contrasting statements to help determine what’s most important to the patient; the second segment let the patient compare the pros and cons of available screening options; and the third segment let the patient decide to have mammograms only, or with MRI included.²
After using the tool, 11 of the 16 women who were originally undecided opted in favor of receiving the additional breast MRI screening. And of the women who had already decided before using the tool, all stayed with their initial decisions. The authors concluded that these promising results produced by the diagnostic aid warrant further study.
Problem-Solving Breast MRI
In a recent publication in RadioGraphics, problem-solving breast MRI was found to be of value when other imaging modalities or physical exams produced inconclusive results. For example, when uncertain imaging findings resulted after mammography and/or ultrasound tests were completed, problem-solving breast MRI was found to be helpful.³
These problem-solving breast MRI exams assist in evaluating challenging situations, such as suspicious nipple discharge or skin changes—suspected to represent an abnormality—or when conventional imaging results were shown to be negative for malignancy. The authors concluded that as deep learning continues to improve, so will the accuracy and value of these problem-solving breast MRI exams.³

The individuals who appear are for illustrative purposes. All persons depicted are models and not real patients or healthcare professionals.
Abbreviated MRI Protocols
Finally, in a symposium presented at RSNA 2023, Margarita Zuley MD, FACR, FSBI, presented her findings from the University of Pittsburgh Medical Center regarding the use of abbreviated MRI protocols for women seeking supplemental breast MRI screenings.4
In her experience, Dr Zuley has found that while full protocol breast MRI is an important screening method for at-risk women, abbreviated breast MRI protocols can increase patient comfort and decrease costs, all while maintaining efficacy and efficiency.4
In addition, Dr Zuley noted that with abbreviated MRI protocols, the reduction of gadolinium dose is important, especially for patients who may require repeat exams, such as women undergoing multiple breast screening examinations.
References:
1. Monticciolo DL, Newell MS, Moy L, Lee CS, et al. Breast cancer screening for women at higher-than-average risk: updated recommendations from the ACR. J Am Coll Radiol. 2023 Sep;20(9):902-914.
2. Chu, C., Smith, C.E., Gorski, J. et al. Implementation of a novel patient decision aid for women with elevated breast cancer risk who are considering MRI screening: a pilot study. Ann Surg Oncol. 2023 Oct;30(10):6152-6158.
3. Reig B, Kim E, Chhor CM, Linda Moy, et al. Problem solving breast MRI. Radiographics. 2023 Oct;43(10):e230026.
4. Zuley M. Breast MRI. Lecture presented at: RSNA; November 27, 2023; Chicago, IL.

